Clinical Information
Overview of the Montreal Model
Feel Emotions, Defuse Thoughts, Change Behaviours
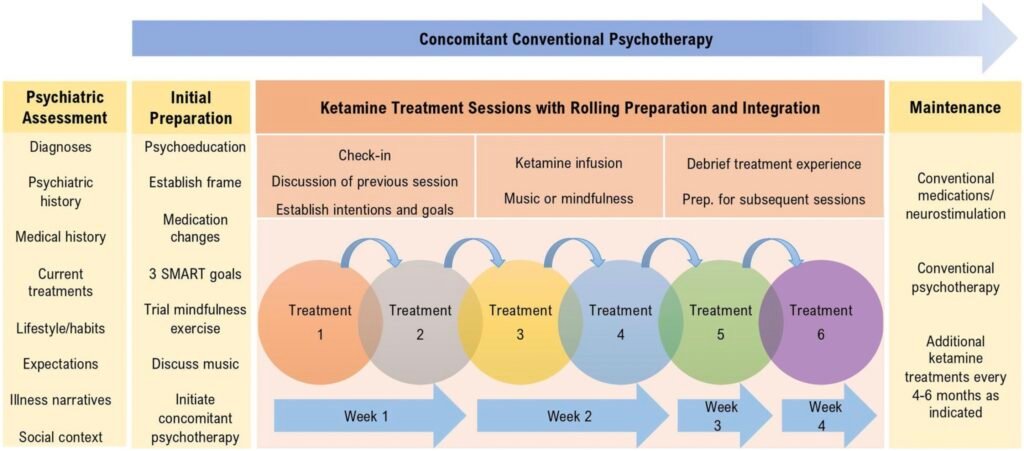
The Montreal Model of Ketamine Therapy is an intensive, evidence-based program that combines low-dose ketamine treatments with psychological support and behavioral changes to help patients recover from treatment-resistant depression. It aims to use the rapid but often temporary antidepressant effects of ketamine as a window of opportunity that, in synergistic combination with psychotherapy and psychedelic-like treatment settings, can facilitate lasting psychological growth and recovery.
Ketamine Treatments
Although originally developed with a standard course of six ketamine treatments over four weeks, the protocol has become more flexible with time depending on a given patient’s needs and contexts. Most will receive 4 or 5 low-dose ketamine treatments over 4 to 6 weeks. These sessions are provided in supportive settings with psychological care to help patients derive psychological growth from the psychedelic-like experiences induced by ketamine.
Each treatment session lasts about 2 hours. It includes a check-in, including a review of previous session experiences, symptoms, and goals. All sessions also include a mindfulness exercise based on Acceptance and Commitment Therapy prior to the ketamine administration (intravenous or intramuscular).
Patients wear blindfolds and can choose to listen to specially curated music playlists or receive guided mindfulness during the 40-minute psychoactive period of the ketamine experience. Medically trained staff are present throughout, monitoring vital signs and providing support for any challenging experiences or side effects.
Evidence-based Behavioural Changes
A key focus of the Montreal Model is to reverse the “vicious cycles” of depression: the negative changes that depression invariably causes that in turn worsen depressive symptoms.
Before the first ketamine treatment, patients work with clinicians to establish at least three clear, specific, measurable, actionable, realistic, and time-based (SMART) behavioral goals. These goals might involve daily routines, diet, exercise, or engaging in meaningful activities. The emphasis is on actionable goals, like “go for a walk every morning,” rather than non-actionable ones like “feel better,” as the former are within the patient’s control.
Psychotherapy
Patients engage in at least one hour of weekly psychotherapy with a qualified professional throughout the ketamine treatment process. This psychotherapeutic support typically begins a few weeks before the first ketamine dose and may continue afterward, serving to help the patient explore thoughts, feelings, and experiences that arise during the ketamine treatments and in their efforts to make life changes.
In the Montreal Model, the specific form of this psychotherapy is flexible – a strong patient-therapist connection is considered more important than the particular therapeutic modality.
Approaching Ketamine Sessions
Patients are encouraged to approach ketamine experiences with curiosity, viewing them as opportunities to explore their inner world and learn. The model encourages resisting the urge to label experiences as “good” or “bad,” and instead to treat all experiences as valuable sources of information and potential growth, even difficult emotions or thoughts.
Indeed, a core principle of the model is that “experiential avoidance” is common to all psychiatric disorders. I.e., that all human beings make efforts to avoid experiencing certain feelings or thoughts in order to reduce our distress, but that this process often actually worsens our suffering in the medium and long-term. In contrast, facing our challenging emotions is often difficult but can yield major benefits.
Music
Specially developed music playlists are available to help make ketamine experiences meaningful and well-tolerated. Patients can choose from these playlists or bring their own music. After treatment, patients are encouraged to re-listen to the music to help integrate their experiences into daily life, a practice many find helpful for solidifying insights.
Side Effects
Common side effects of low-dose ketamine include psychedelic-like or dream-like experiences (dissociation), dizziness, nausea, vision changes, drowsiness or excitement, elevated blood pressure and heart rate, increased salivation, and involuntary muscle movements. Most side effects are brief and resolve within a couple of hours. Medications can be provided for bothersome side effects like nausea.
Post-Treatment Care
After a ketamine session, patients cannot drive for 24 hours or until after a restful night’s sleep. They are encouraged to continue working on their behavioral goals and with their psychotherapist. Patients can contact the clinical team for any concerning symptoms or go to an emergency room for urgent issues.